From Eradication to Epidemic: The Return of Measles
Overview of Measles and Its Impact
Measles is recognized as one of the most contagious viral diseases, posing serious health risks, particularly to unvaccinated individuals, young children, and those with weakened immune systems. The virus is primarily spread through respiratory droplets, which are expelled when an infected person coughs or sneezes. Additionally, it can be contracted by touching surfaces contaminated with these droplets, highlighting the ease with which measles can be transmitted. Remarkably, the virus can persist in the air for up to two hours after an infected person has left, underscoring its potential for rapid and widespread transmission.
Though measles was declared eliminated in the United States in 2000, the reality is that outbreaks still occur. These outbreaks are often fueled by unvaccinated travelers who bring the virus from other countries, illustrating the global interconnectedness of health issues. The resurgence of measles globally, particularly in areas with low vaccination coverage, highlights the critical need for maintaining high immunization rates. For example, countries with declining vaccination rates have reported significant increases in measles cases, stressing the importance of herd immunity in preventing widespread outbreaks. As such, ensuring robust vaccination coverage remains a pivotal strategy in controlling measles and safeguarding public health.
Symptoms and Early Signs
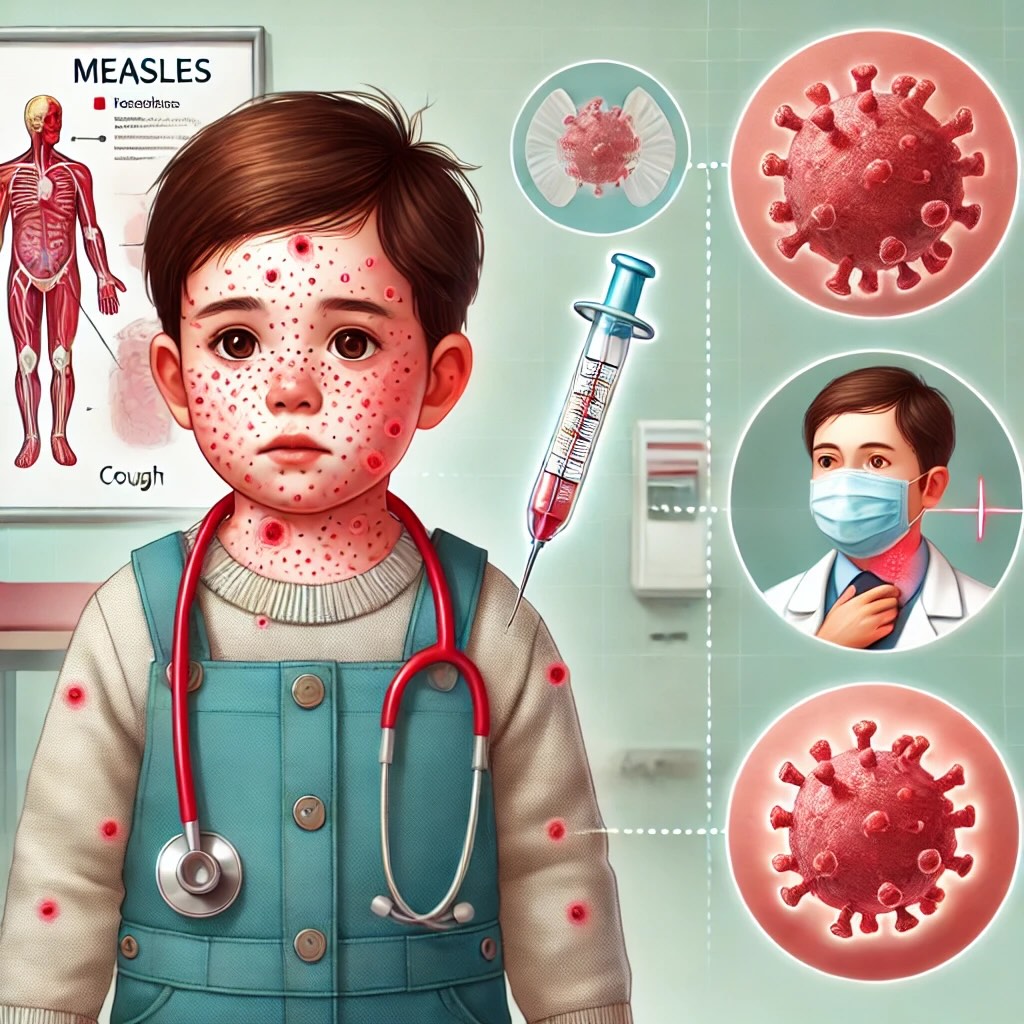
Measles symptoms typically manifest 7 to 14 days after exposure, beginning with a prodrome of high fever, cough, runny nose, and red eyes, which are indicative of the disease’s onset. These early symptoms can be mistaken for a common cold or other viral infections, making it crucial to monitor any progression, especially in young children who are more vulnerable to complications. A child may initially display a high fever and general malaise, which should prompt parents to be vigilant for further developments.
As the illness progresses, a characteristic maculopapular rash emerges, starting on the face and spreading systematically to the trunk and limbs, marking a definitive indicator of measles. Alongside the rash, Koplik spots—small white lesions with a bluish-white center found inside the mouth—appear and are considered a hallmark diagnostic sign for healthcare professionals. While children under the age of five are at a heightened risk for severe complications such as pneumonia and encephalitis, adults, too, can suffer from significant health risks, potentially leading to hospitalization. For example, an adult might experience milder symptoms initially, but without proper care, the disease can escalate, underscoring the importance of early detection and medical consultation.
Complications and Risks
Measles is a formidable virus that can result in a range of severe complications, with pneumonia and encephalitis being among the most concerning. Encephalitis, an inflammation of the brain, can lead to long-term neurological damage, profoundly affecting an individual’s quality of life. The lethality of measles is notable, as approximately three out of every 1,000 children infected succumb to these complications. This high mortality rate underscores the potential dangers of the virus, especially for vulnerable populations such as infants and young children, who are particularly susceptible to severe outcomes like blindness and respiratory diseases.
The risk of pneumonia in children with measles is significant, with about one in 20 developing this potentially life-threatening condition. Pneumonia poses a grave threat to young patients, often necessitating hospitalization and intensive medical care. Moreover, diagnosing and treating measles in immunocompromised individuals presents unique challenges since they might not exhibit the typical symptoms, further complicating the clinical approach. This variability in symptoms calls for heightened vigilance among healthcare professionals to ensure timely and accurate diagnosis and intervention, particularly in high-risk groups.
Importance of Vaccination
Vaccination against measles is crucial in safeguarding public health, with the MMR (measles, mumps, rubella) vaccine proving to be the most effective preventive measure. This vaccine boasts a remarkable 97% efficacy rate after two doses, underscoring its effectiveness in protecting individuals from measles. To establish herd immunity and effectively prevent outbreaks, it is essential to maintain a vaccination rate of at least 95% within the community. Unfortunately, vaccine coverage has waned in some regions due to misinformation and hesitancy, posing a significant risk to public health.
The historical context further emphasizes the importance of vaccination. Before the vaccine became available, measles was rampant in the United States, with an estimated 3 to 4 million infections annually, leading to numerous hospitalizations and fatalities. However, since its introduction, the MMR vaccine has played a pivotal role in saving countless lives by averting over 60 million deaths globally, highlighting its indispensable role in combating measles. The decline in vaccination rates in certain areas necessitates renewed public health efforts to educate communities and dispel myths surrounding vaccines, ensuring sustained protection against measles for future generations.
Diagnosis and Prevention Strategies
Healthcare professionals diagnose measles primarily through a careful clinical evaluation of symptoms, such as the presence of Koplik spots in the mouth, which are a distinctive feature of the disease. This evaluation is often supplemented by laboratory tests that can provide a definitive confirmation of the virus. Laboratory testing typically involves serological assays to detect measles-specific IgM antibodies or the isolation of the measles virus RNA from a patient’s blood or throat swabs. These diagnostic methods are essential for confirming cases, particularly in the early stages of an outbreak, when the rapid spread of the virus can overwhelm communities.
Preventive strategies are equally critical in controlling measles. The cornerstone of measles prevention is vaccination, specifically the administration of the MMR vaccine. This vaccine is highly effective, with two doses providing a 97% efficacy rate in preventing measles. It is recommended that children receive the first dose of this vaccine between 12 to 15 months of age and the second dose between 4 to 6 years of age. In addition to vaccination, isolating suspected measles cases and ensuring that hygiene practices, such as regular hand washing and proper respiratory etiquette, are followed can significantly reduce transmission. Public health campaigns play a vital role in educating communities about the importance of these preventive measures. These campaigns often focus on dispelling myths and misinformation surrounding vaccines, such as the debunked claim linking vaccines to autism. During outbreaks, health authorities act swiftly by setting up immediate vaccination clinics to increase immunization rates and contain the spread of the virus. These clinics are strategically located in affected areas to maximize accessibility and impact.
 The West Texas Outbreak
The West Texas Outbreak
The measles outbreak in West Texas has reached a concerning magnitude, with 90 confirmed cases reported mainly among individuals who have not been vaccinated. This surge in cases is particularly concentrated in communities with historically low vaccination rates, such as the Mennonite population, highlighting the critical role of vaccination in disease prevention. The outbreak underscores the importance of achieving herd immunity to prevent such occurrences. Public health officials are emphasizing the urgent need for increased vaccination efforts and are working to raise awareness about the risks of measles and the protective benefits of the MMR vaccine.
Reports have highlighted that a significant percentage of kindergartners in the affected areas remain unvaccinated, exacerbating public health concerns and increasing the potential for further spread of the virus. In response, local health departments have mobilized efforts to collaborate with schools and community organizations, aiming to promote vaccination and dispel any vaccine-related myths that contribute to hesitancy. These efforts include setting up immediate vaccination clinics to increase immunization rates and deploying educational campaigns to inform the public about the severity of measles and the critical importance of vaccination in preventing outbreaks.



